CITE THIS WORK
Sánchez Moreno S, Diéguez Castillo C. Type 1 autoimmune pancreatitis: a diagnostic challenge with an atypical presentation. RAPD 2025;48(2):82-84. DOI: 10.37352/2025482.6
Introduction
We present the case of a 51-year-old man diagnosed with autoimmune pancreatitis type 1 based on clinical and serological criteria with unusual radiological findings that pose an added difficulty to the differential diagnosis of pancreatic inflammatory pathology.
Clinical case
A 51-year-old male patient with a history of type 2 diabetes mellitus and dyslipidemia came to the emergency department for 48 hours of pain in the right hypochondrium radiating to the back and oral intolerance, with associated weight loss, without jaundice or fever. Blood tests on arrival showed creatinine 1.5 mg/dL, albumin 3g/dL, hemoglobin 11 g/dL, CRP 12 mg/dL and leukocytosis with neutrophilia; amylase, total bilirubin and the rest of the liver profile were normal.
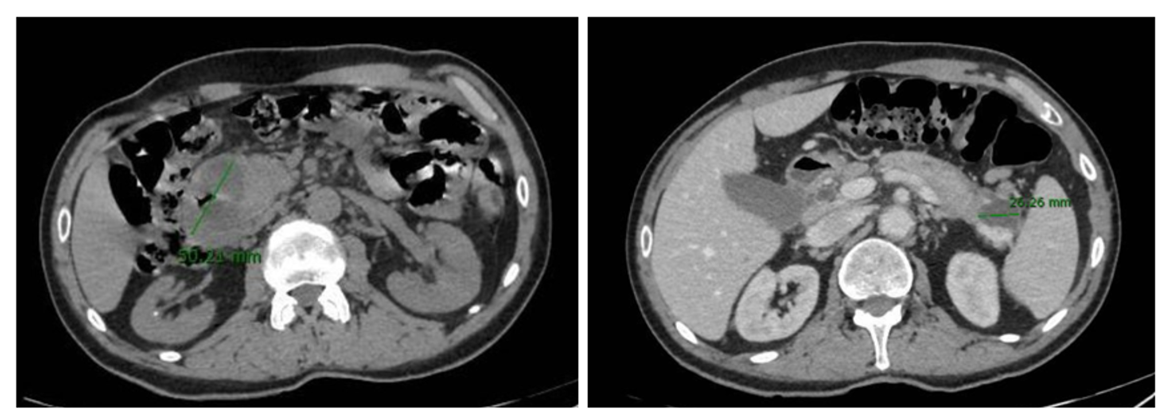
An abdominal CT scan with contrast was performed with findings suggestive of an inflammatory process at the pancreaticoduodenal junction, without being able to rule out underlying tumor etiology, with several associated pancreatic collections, the largest of about 5 cm, which produced obliteration of the first duodenal portion and ectasia of the extrahepatic biliary tract, with associated locoregional lymphadenopathy (Figure 1).
The tumor marker CA 19.9 was normal, and an echoendoscopy was performed (unable to progress to the second duodenal portion due to extrinsic compression) suggesting the cystic origin of the previously described pancreatic lesions with a homogeneous enlargement of the pancreas without other focal lesions, which points to the inflammatory origin of the picture.
Serologic analysis detected an elevated immunoglobulin G (2090 mg/dL; VN 700-1600 mg/dL) with IgG4 of 1110 mg/d (>2 times the VLSN). Subsequently the study was completed with an MRI that showed a diffuse enlargement of the pancreas with peripheral hypointense halo and collections of liquid content, suggesting an autoimmune pancreatitis given the clinical and analytical context of the patient (Figures 2 and 3).
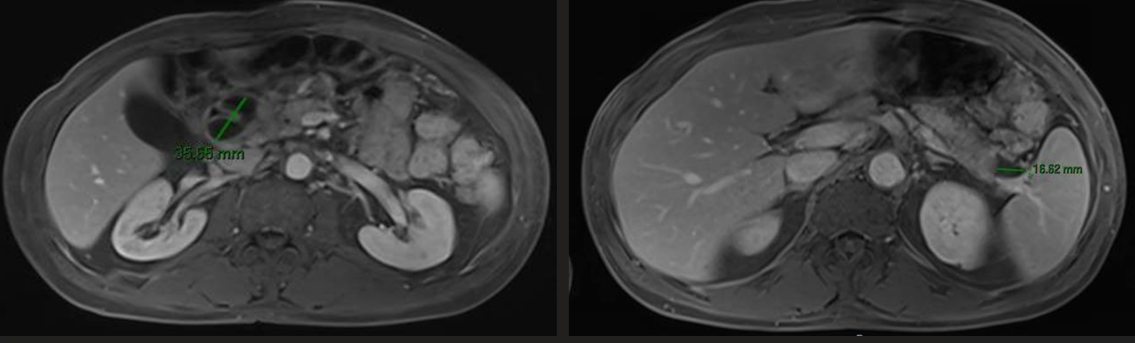
Figure 2
Abdominal MRI. Decrease in size of pancreatic collections after initiation of steroid treatment.
Treatment with corticosteroids was started and the patient showed clinical improvement with progressive oral tolerance and favorable radiological findings after two weeks, with a decrease in the size of the pancreatic collections as well as the locoregional lymphadenopathies.
Discussion
Autoimmune pancreatitis (AIP) refers to a chronic inflammatory and fibrosing disease of the pancreas, of benign behavior and autoimmune origin, with response to treatment with corticosteroids.
Type 1 IAP can be considered as a pancreatic manifestation within the spectrum of IgG4 diseases and the involvement of other extra-pancreatic organs is frequent, while in type 2 IAP there is usually no serum elevation of IgG4 and it can be related to inflammatory bowel disease[1].
Currently, the criteria most commonly used to make the diagnosis of autoimmune pancreatitis are those of the International Consensus (2011), based on histology, radiological findings, serum IgG4 levels[2], involvement of other extra-pancreatic organs and response to corticosteroid treatment. Depending on their combination, the probable or definitive diagnosis of IAP can be established[3].
While type 1 IAP can be diagnosed with high accuracy without pancreatic biopsy, a diagnosis of type 2 IAP almost always requires histologic confirmation. In our case, the presence of compatible radiological findings together with significant elevation of IgG4 levels and a favorable response to corticosteroids allowed us to make the diagnosis of type 1 IAP with high accuracy.
The main differential diagnosis of IAP should be established with pancreatic adenocarcinoma since the clinical features of the disease (constitutional syndrome, obstructive jaundice, vomiting and oral intolerance) and the radiological findings (diffuse or focal pancreatic enlargement) often raise the suspicion of a pancreatic neoplasm. In fact, a not inconsiderable percentage of patients undergoing duodenopancreatectomy for suspected cancer are eventually diagnosed with PAI[1]. It is also important to include in the differential diagnosis of IAP other neoplasms that can affect the pancreas, such as neuroendocrine tumor and pancreatic lymphoma.
On the other hand, the presence of acute collections and pseudocysts in IAP has classically been described in the literature as an infrequent finding that can contribute confusion to the diagnosis; nevertheless, in recent years some series have been published indicating that the incidence of these lesions in patients with IAP can be between 9.7% and 22.4%[4],[5]. The appearance of pancreatic cystic lesions in the setting of autoimmune pancreatitis seems to be related to local inflammation of the pancreatic segments affected by the disease together with stenosis of the intra-pancreatic bile ducts that can lead to secondary retention of pancreatic secretion. Generally these lesions affect the pancreatic body and tail[5], can be single or multiple and, on very rare occasions, of hemorrhagic or necrotic content, sometimes simulating a pancreatic cystic neoplasm[6]. In our case, the elevated levels of immunoglobulin G were decisive in guiding the diagnosis.
The appearance of pancreatic cystic lesions in a synchronous manner is one of the particularities of our case, as well as the duodenal compression secondary to the largest lesion (> 3cm) with manifest clinical repercussions in our patient, with impossibility of oral intake and significant improvement after the initiation of corticosteroids.
With our case we want to highlight the importance of considering IAP in the differential diagnosis of pseudocyst and acute pancreatic collections[7], and we provide evidence in favor of early management of these lesions in IAP with corticosteroid treatment given the high rate of regression after its onset, being more exceptional the surgical approach in these cases.

 Descargar número completo
Descargar número completo Download full issue
Download full issue