CORRESPONDENCE
Eduardo Adán Baute Trujillo
University Clinical Hospital San Cecilio. Granada.
18007 Granada
Cite this work
Baute Trujillo EA, Librero Jiménez M, Martínez Tirado P, Moreno Barrueco M. Cholecystoduodenal fistula: a rare cause of intestinal obstruction, an extraordinary cause of hematemesis. RAPD 2025;48(4):146-148. DOI: 10.37352/2025484.6
Introduction
Cholecystoenteric fistulas are a rare complication of gallstone disease. They are associated with ischemia and inflammation, which cause erosion and ultimately fistulization of the gallbladder wall. Among these, cholecystoduodenal fistulas are the most prevalent, with highly variable clinical presentation. In most cases, they are asymptomatic and are diagnosed incidentally during imaging tests or abdominal surgery; however, they can also occur, less frequently, in the form of recurrent cholangitis or pancreatitis, abscesses, intestinal obstruction due to biliary ileus, or, exceptionally, in the form of gastrointestinal bleeding[1]. With regard to biliary ileus, it should be noted that the terminal ileum is the most common site of impaction, but sometimes the stones become lodged in more proximal sections such as the jejunum or duodenum, causing gastric obstruction known as Bouveret's syndrome[2].
Clinical case
We present the case of a 70-year-old foreign patient with a personal history of chronic kidney disease on renal replacement therapy, symptomatic cholelithiasis, and abdominal surgery for which no reports are available. He came to the emergency room with epigastric pain and hematemesis with hemodynamic instability. Laboratory tests showed hemoglobin of 7.5 g/dL (previous 12.8 g/dL) along with worsening of baseline renal function with creatinine at 9.2 mg/dL. A gastroscopy was performed, which revealed upper gastrointestinal bleeding secondary to a duodenal ulcer of inflammatory origin, probably in the context of a foreign body, suggesting gallstones lodged at that level. An attempt was made to remove it, but this was unsuccessful, revealing an ulcer with an adherent clot and congestive edges without active bleeding in the underlying mucosa (Figure 1).
Figure 1
Upper gastrointestinal endoscopy image showing gallstones lodged in the duodenum, revealing an ulcer with an adherent clot and congestive edges in the underlying mucosa.
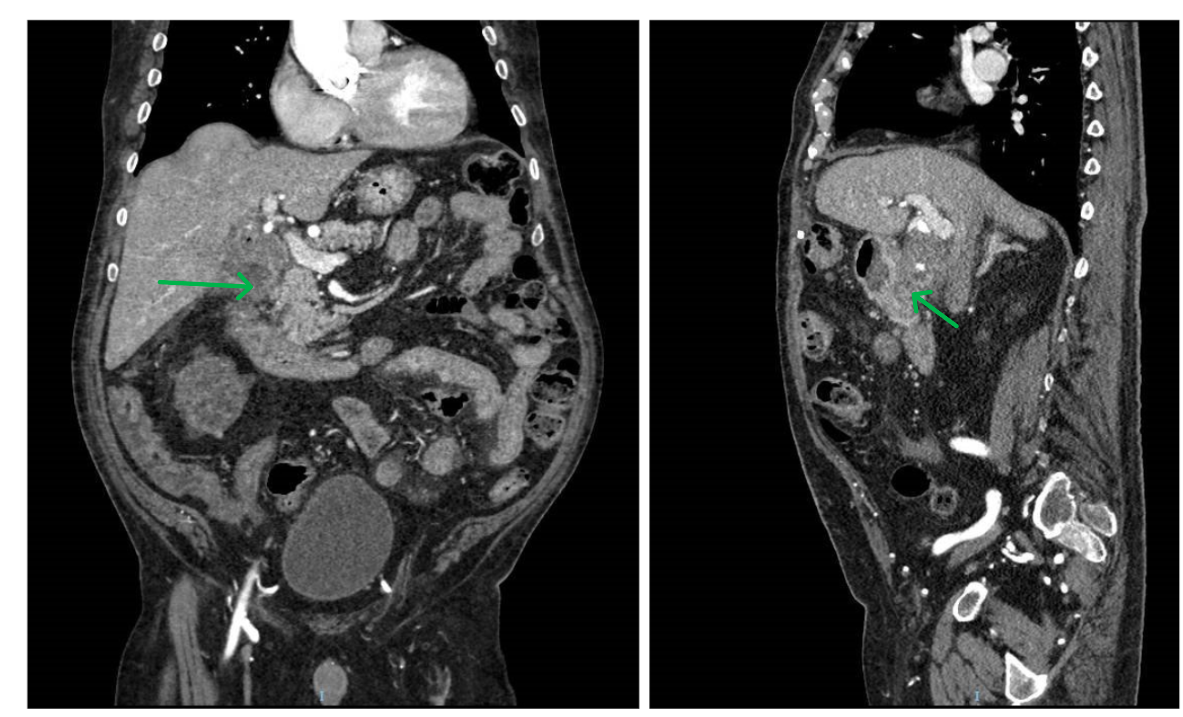
A CT scan of the abdomen was then performed due to suspicion of a cholecystoduodenal fistula. This imaging test reveals an 8 mm cholecystoduodenal fistula with air bubbles in the vesicular lumen and rarefaction of the perivesicular and periduodenal fat, without the duodenal lithiasis described in the endoscopy, together with an extraluminal contrast focus in the wall of the gallbladder, probably due to a small aneurysm (Figure 2).
Figure 2
Coronal and sagittal CT scans of the abdomen with initial contrast, showing an 8 mm cholecystoduodenal fistula with rarefaction of fat adjacent to the gallbladder and duodenum.
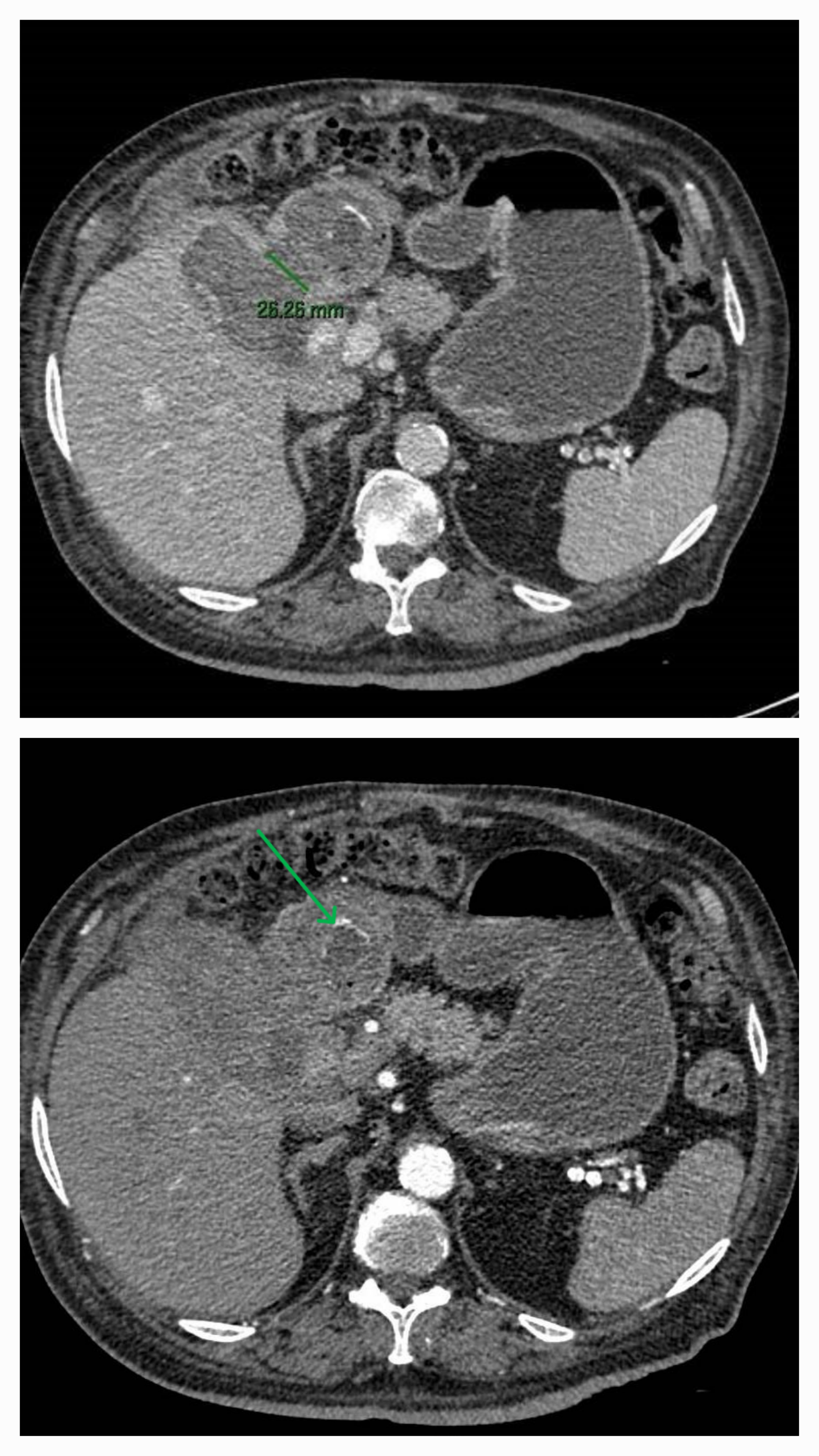
Figure 3
Bouveret's syndrome secondary to passage of a 2.6 cm cholelithiasis to the first portion of the duodenum through a cholecystoduodenal fistula that has increased significantly in size. Occupation of the gastric chamber and first and second portions of the duodenum by blood material.
The patient is discharged pending scheduled surgery, but returns a few weeks later with epigastric pain and vomiting with hemodynamic instability. A new abdominal CT scan is performed with findings that are compatible with Bouveret's syndrome secondary to cholelithiasis in the first portion of the duodenum due to a known cholecystoduodenal fistula that had increased significantly in size. He also presented with dilation of the gastric chamber and the first and second portions of the duodenum, which were occupied by hyperdense material suggestive of blood, with an active bleeding point observed on the wall of the gallbladder (Figures 3-4).
Figure 4
Active bleeding point in the gallbladder wall near the infundibulum, in the area where a small pseudoaneurysm was described in the previous CT scan.
Based on the above, the patient underwent open cholecystectomy, with hemostasis of the aneurysmal bleeding and removal of the duodenal gallstones. He was subsequently discharged after treatment with empirical antibiotic therapy and good progress.
Discussion
The clinical presentation of a cholecystoduodenal fistula in the form of upper gastrointestinal bleeding, although well described in the literature, is a very rare finding. Invasion of the cystic artery by a duodenal ulcer can cause massive bleeding, and a gallstone can cause erosion of the same artery, thus causing bleeding. In the review conducted by Park JM et al., endoscopic hemostasis was attempted in up to 4 of the cases described, but surgery was ultimately necessary in all of them[3],[4]. In summary, gastrointestinal bleeding caused by a cholecystoduodenal fistula usually requires surgery, as it is unlikely that the bleeding will resolve with conservative treatment or endoscopic hemostasis.
On the other hand, the fact that this same patient subsequently developed Bouveret's syndrome is unusual. As in our case, the definitive treatment for this complication is surgical, although there is no consensus on the appropriate surgical procedure. The most commonly used procedure is enterolithotomy with open cholecystectomy, given the chronic inflammation and anatomical distortion[1],[2].
In conclusion, cholecystoduodenal fistulas should be considered in the differential diagnosis when a patient with a history of biliary disease presents with gastrointestinal bleeding.

 Descargar número completo
Descargar número completo Download full issue
Download full issue